What is periodontitis?
Periodontitis, or gum disease, is a serious infection of the gum that damages the supporting tissues of the teeth. If it progresses, it can cause significant damage to both gum tissues and bone structures where teeth are anchored (periodontal ligament and alveolar bone). Periodontitis is mainly caused by poor oral hygiene, which increases the risk of bacterial activity in dental plaque.
Periodontitis is common but it is preventable. You can simply brush your teeth twice a day, floss daily, and have regular dental visits to greatly improve your oral health and minimize risks of gum disease development. It is highly important to visit your dentist to prevent and stop gum disease in the early stages since the damage caused by periodontitis can be irreversible.
What are the symptoms of periodontitis?
As gingivitis precedes periodontitis, knowing the symptoms of gingivitis can set an alarm to prevent serious gum disease occurrence. You can notice changes like:
- Red and swollen gums
- The existence of plaque and tartar buildups on teeth
- Bleeding in gums that can happen spontaneously or when triggered by eating or brushing teeth
- Receding gums in which your teeth look longer
- Bad breath
- Loose teeth
- Pain or sensitivity
- Recurrent inflammation in gums
Your dentist can detect any high-risk signs and symptoms that are present in your gums or teeth even during the early phases. Before things go too far, seek your dentist’s help and, if diagnosed, receive the necessary treatments.
What causes periodontitis?
To make it simple, periodontitis is caused by the buildup of bacterial plaque that is the result of lack of proper oral hygiene. Our mouth is full of hundreds of species of bacteria. Although some of these bacteria don’t cause any harm, others can build up to form dental plaque, which colonize the surface of teeth. If you don’t brush your teeth and don’t remove the accumulated plaque, it turns into harder deposits of bacterial plaque, called calculus or tartar.
The most common risk factors that reinforce and increase the risks of developing periodontitis include:
1. Smoking
Tobacco use or smoking habits are the biggest risk factors for gum disease. In smokers, there is a favorable environment for bacteria to breed and form gum pockets and periodontitis advances with a higher speed. Bear in mind that treatments are also more difficult for smokers than non-smokers. There are even higher risks of not responding to periodontal treatment in individuals who smoke.
2. Type 2 diabetes
People who are suffering from diabetes are at a greater risk of developing periodontal diseases. Changes in blood sugar level should be managed to prevent gum problems. It is important to visit the dentist to do periodontal examination for possible gingivitis signs and symptoms.
3. Genetics
Periodontitis is directly linked to the interplay between bacterial infection and the immune system. Individuals with systemic diseases or certain syndromes and disorders can be susceptible to the way the body reacts to the progression of gum diseases.
4. Poor diet and nutritional deficiencies
The negative eating habits and consumption of unhealthy foods such as processed food, diets high in sugar, soft drinks, and carbohydrate-rich diet are well-known causes of tooth decay. This helps bacterial plaque to thrive and hence pave the way for gingivitis or gum inflammation. Some types of deficiencies like vitamin C shortages are linked to gingivitis. Therefore, poor diet not only is an issue for teeth but a reinforcer for more gum problems.
5. Age
Periodontal diseases can start at early adulthood or even earlier but may take years to progress. As we age, longtime untreated diseases, poor oral hygiene, and many other factors exacerbate gum disease. Chronic periodontitis appears to cause immense damage especially when people reach higher ages, like older than 35 years of age.
Other risk factors include:
- Stress
- Medications used like those that interrupt saliva function and cause dry mouth
- Hormonal changes during pregnancy, menopause and other situations
- HIV or other compromised immune system conditions
What are the stages of periodontitis?
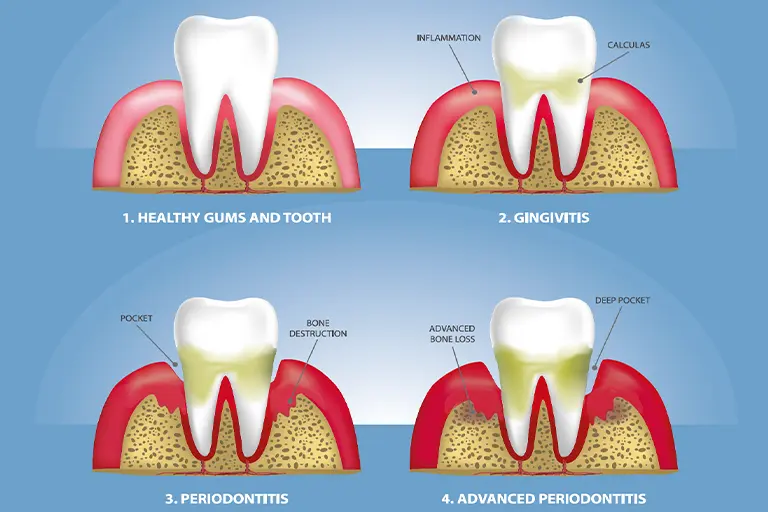
Early stage of periodontal disease (gingivitis)
At the beginning of gum disease, individuals show signs of gingivitis, which is the milder form of gum disease and is characterized by redness, inflammation and bleeding gum problems. Gingivitis then leads to periodontitis (periodontal disease) if it is not treated.
The most common cause of gingivitis is poor oral hygiene. With increasing risks of dental plaque, many species of bacteria living in the unremoved plaque and in your mouth find the chance to harm your teeth and gums. If you don’t brush your teeth and have no regular flossing, this gives rise to bacterial plaque and therefore a growing risk of infections, which results in gingivitis.
Once periodontitis occurs, you can expect irreversible and serious damage to gums, teeth, and the connective tissues that support your teeth. Chronic periodontitis is divided into three stages:
Mild periodontal disease
At this stage of periodontitis, attachment loss has occurred, meaning that connective tissues (gingival fibers and periodontal ligament) in contact with tooth roots become detached. Gums recede and teeth appear longer than normal. Pockets with smaller depth begin to form between gums and teeth and there is an increasing bacterial infection, which may give you a foul odor in your mouth.
Moderate periodontal disease
As the periodontitis goes untreated, the damage becomes more significant. The connective tissue and the alveolar bone are destroyed, leading to loose teeth. Receding gums, bleeding, bone loss, and deeper periodontal pocket cause irreversible damages that require long-term care and treatment.
Advanced periodontal disease
It is extremely important to prevent further progression of periodontitis as soon as possible. In the advanced periodontitis stages, the disease may get unresponsive to treatment or recur again and again. The connective tissue, gums, and supporting bone get so severely damaged that tooth loss will be even more likely. Thus, the destruction of attachment tissues and the high level of tooth mobility eventually lead to tooth loss.
What are treatments for periodontitis?
Depending on the periodontitis condition, treatments aim to eliminate the infection in pocket gums and improve the affected gum or bone structures. If the periodontitis is in the early stages, you may be asked to best manage your oral health at home along with treatments at dentists’.
Common treatments of periodontitis include:
Maintaining oral hygiene
Your dentist can instruct you or remind better teeth cleaning ways and the importance of oral hygiene. Your dentist will guide you on ways to remove plaque better and prevent the growth of bacteria in your mouth.
You may be required to use the right toothbrush, the appropriate toothpaste and the antibacterial mouthwashes. Your dentist will advise on:
- Brushing teeth twice a day or even better after snacking
- Changing your toothbrush (e.g., every 3 months)
- Using an electric toothbrush or a suitable form of toothbrush designed for easier interdental or posterior teeth cleaning to clean teeth of plaque and tartar formed on hard-to-reach spots
- If recommended, using antiseptic mouthwashes to treat gum infection and inflammation
- Medication use especially those that directly impact oral functions such as saliva problems
- Trying healthier lifestyle such as quitting smoking, cutting down on high-sugar foods/drinks, and avoiding carbonated and acidic beverages
Tooth scaling and root planing
Scaling is done to scrape off plaque from the surface of teeth which you can’t remove with toothbrushing alone. Your dentist can use ultrasonic instruments, laser or other necessary dental instruments to do scaling. With root planing the lower root area of teeth, after removal of plaque, is smoothed to prevent bacteria buildups from residing on the tooth root below the gum line areas. They can remove plaque buildups and calculus (tartar) that are formed on teeth’s surface or the exposed spots below the gums.
Fluoride treatment (fluoride varnish)
Fluoride is a well-known ingredient used in toothpaste, which helps strengthen teeth and fight caries. They will apply higher concentration of fluoride on teeth to speed up plaque elimination in a much more efficient way.
Antibiotic therapy
Sometimes, oral hygiene regimen may not be enough. Your dentist can prescribe antibiotic medications to prevent further risks of persisting gum infections.
Surgery
If the periodontitis has caused serious damage to bone and gums and the periodontal pocket is deeper, your dentist or periodontist will decide on the surgeries as treatment. They can perform:
- Flap surgery
-
This surgery is done because the dentist or periodontist needs to get access to teeth in deeper pockets for scaling and root planing (debridement). Therefore, gums are lifted back, the bacterial deposits are cleaned along with scaling and planing of tooth roots. If required, the supportive underlying bone structures is recounted. Then the gum tissues are sutured back.
- Bone grafting
-
Sometimes due to bone defects caused by periodontal issues, dentists or periodontists need to regenerate the lost bone structures. This way, they will use the bone grafts from your own bone or the donated bone graft to generate bone tissue regrowth in the site of periodontal pocket.
Your dentist or periodontist can also help the defective bone to grow using the method called interdental denudation or guided tissue regeneration. After the excision of the gum tissues in the interproximal area between teeth and bone, it is covered with some form of periodontal dressing to allow for the healing of the bone.
- Gum grafting
-
One of the notable symptoms of periodontitis is receding gum issues that can be treated through surgical operation. Dental specialists will treat this complication through gum grafting. This surgery allows for lost gum tissues to regenerate. The healthier soft tissue that is taken from other oral tissues (e.g., roof of the mouth) is inserted in the place of gum recession area.
How to prevent periodontitis?
You can prevent chances of periodontitis development by following below hygiene tips:
- Brush your teeth twice a day to remove plaque buildups on your teeth
- Brush interdental spaces carefully or use helpful oral care products to make brushing easier such as electric toothbrushes, dental picks or other specially designed products
- Floss daily
- Use fluoride toothpaste to strengthen teeth while fighting tooth decay and preventing cavities
- Try antiseptic mouthwashes to kill bacteria when recommended by your dentist
- Limit your sugar intake and eat/drink healthier
- Avoid smoking and using tobacco
- Most importantly, visit your dentist regularly to have your teeth examined for possible signs and symptoms or maybe for professional teeth cleaning appointment for better plaque removal.
Frequently asked questions
While gingivitis is gum inflammation that affects the gum line and other surrounding gum tissues, periodontitis goes beyond the soft tissues of the gums and damages bones that anchor teeth in place.
Gingivitis can be reversed and you can restore your gum health with good oral hygiene practices. But once periodontitis comes in, oral hygiene alone is not enough because of adverse destruction of the gums and periodontium. The repair of the damages caused needs a dentist or a periodontist’s treatment and care.
Your dentist or periodontist (the dentist specializes in treating periodontal diseases) will diagnose the existence of periodontitis through periodontal probe for the presence of periodontal pocket or through diagnostic images. These measurements and radiographic images allow dentists to easily detect or notice signs of bone loss, infections, and other periodontal conditions in gums and surrounding bony structures.
